Diabetic Peripheral Neuropathy
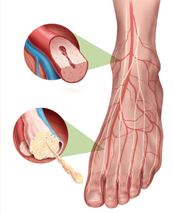
Diabetic neuropathy is nerve damage caused by diabetes. When it affects the arms, hands, legs and feet it is known as diabetic peripheral neuropathy. Diabetic peripheral neuropathy is different from peripheral arterial disease (poor circulation), which affects the blood vessels rather than the nerves. with pain medication or pain killers. Diabetic peripheral neuropathy doesn’t emerge overnight. Instead, it usually develops slowly and worsens over time. Some patients have this condition long before they are diagnosed with diabetes. Having diabetes for several years may increase the likelihood of having diabetic neuropathy.
Depending on the type(s) of nerves involved, one or more symptoms may be present in diabetic peripheral neuropathy.
For sensory neuropathy:
- Numbness or tingling in the feet
- Pain or discomfort in the feet or legs, including prickly, sharp pain or burning feet
For motor neuropathy:
- Muscle weakness and loss of muscle tone in the feet and lower legs
- Loss of balance
- Changes in foot shape that can lead to areas of increased pressure
For autonomic neuropathy:
- Dry feet
- Cracked skin

